Probiotics May Improve Symptoms of Recurrent Abdominal Pain in Children
Probiotics may alleviate pain in the short-term in children with recurrent abdominal pain (RAP), according to an updated review recently published in the Cochrane Database of Systematic Reviews.1
Up to 25% of children are affected by RAP significantly enough to impinge on their daily life.2 RAP encompasses a range of gastrointestinal disorders (eg, irritable bowel syndrome, abdominal migraine, functional abdominal pain) and often produces symptoms beyond abdominal pain. In most cases, the etiology of RAP is unknown, rendering treatment difficult. In the current study, the researchers conducted a systematic review and meta-analysis of randomized controlled trials that evaluated the effectiveness of a number of dietary interventions aimed at improving RAP symptoms. The most heavily studied intervention was probiotics.
The literature search identified 19 eligible randomized placebo-controlled trials that evaluated the efficacy of one or more dietary interventions in children with RAP. The intervention phase typically spanned 4 to 6 weeks. Cumulatively, the trials enrolled 1453 participants from 8 different countries (all outside the United States), aged 4 to 18 years. Most trials were small, single-institution studies conducted at pediatric gastroenterology clinics.
The efficacy on RAP-associated pain of the following dietary interventions was assessed: probiotics (13 studies, n = 1453); fiber-based interventions (4 studies, n = 299); a low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet (1 study, n =34); a fructose-restricted regimen (1 study, n = 103).
The review's primary objective was to determine whether any dietary intervention reduced the intensity, duration, or frequency of pain. Secondary outcomes included the diet's effect on school performance, social or psychological function, and quality of life.
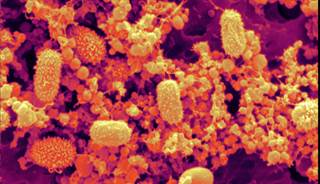
The type of bacteria used in the probiotic trials varied, although most tested a strain of lactobacillus. Overall, children with RAP who were treated with probiotics were more likely than children given placebo to report improvements in pain by 3 months (moderate quality of evidence; odds ratio [OR], 1.63; 95% CI, 1.07-2.47). Children with irritable bowel syndrome were the most likely to have a decrease in pain after taking probiotics (moderate quality of evidence; n = 344; 4 studies; OR, 3.01; 95% CI, 1.77-5.13). Children treated with probiotics were also more likely than those taking placebo to have a reduction in pain frequency (n = 523; 6 studies) and intensity (n = 575; 7 studies) by 3 months, although the level of evidence for these outcomes was low quality. The authors said too few trials provided data on the secondary outcomes to draw meaningful conclusions.
Children treated with fiber-based interventions were no more likely to have improvement in pain at 3 months than those treated with placebo. In addition, fiber-based interventions did not reduce pain intensity. Although meta-analyses of low FODMAP or low fructose diets were not possible, the limited data available from the single studies of these interventions suggested they might offer some benefit, but the authors questioned the quality of the studies.
The researchers concluded that there was “moderate to low quality evidence suggesting that probiotics may be effective in improving pain in children with RAP.” They concluded that “Clinicians may therefore consider probiotic interventions as part of a holistic management strategy,” called for additional studies with improved protocols to evaluate these and other dietary interventions.
Summary and Clinical Applicability
Probiotics may improve pain in children with RAP. Fiber supplements do not appear to be effective. Clinicians may consider probiotics as a management strategy for RAP.
http://www.clinicalpainadvisor.com/abdominal-pelvis-pain/treating-pediatric-recurrent-abdominal-pain-with-probiotics/article/655570/
Up to 25% of children are affected by RAP significantly enough to impinge on their daily life.2 RAP encompasses a range of gastrointestinal disorders (eg, irritable bowel syndrome, abdominal migraine, functional abdominal pain) and often produces symptoms beyond abdominal pain. In most cases, the etiology of RAP is unknown, rendering treatment difficult. In the current study, the researchers conducted a systematic review and meta-analysis of randomized controlled trials that evaluated the effectiveness of a number of dietary interventions aimed at improving RAP symptoms. The most heavily studied intervention was probiotics.
The literature search identified 19 eligible randomized placebo-controlled trials that evaluated the efficacy of one or more dietary interventions in children with RAP. The intervention phase typically spanned 4 to 6 weeks. Cumulatively, the trials enrolled 1453 participants from 8 different countries (all outside the United States), aged 4 to 18 years. Most trials were small, single-institution studies conducted at pediatric gastroenterology clinics.
The efficacy on RAP-associated pain of the following dietary interventions was assessed: probiotics (13 studies, n = 1453); fiber-based interventions (4 studies, n = 299); a low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet (1 study, n =34); a fructose-restricted regimen (1 study, n = 103).
The review's primary objective was to determine whether any dietary intervention reduced the intensity, duration, or frequency of pain. Secondary outcomes included the diet's effect on school performance, social or psychological function, and quality of life.
The type of bacteria used in the probiotic trials varied, although most tested a strain of lactobacillus. Overall, children with RAP who were treated with probiotics were more likely than children given placebo to report improvements in pain by 3 months (moderate quality of evidence; odds ratio [OR], 1.63; 95% CI, 1.07-2.47). Children with irritable bowel syndrome were the most likely to have a decrease in pain after taking probiotics (moderate quality of evidence; n = 344; 4 studies; OR, 3.01; 95% CI, 1.77-5.13). Children treated with probiotics were also more likely than those taking placebo to have a reduction in pain frequency (n = 523; 6 studies) and intensity (n = 575; 7 studies) by 3 months, although the level of evidence for these outcomes was low quality. The authors said too few trials provided data on the secondary outcomes to draw meaningful conclusions.
Children treated with fiber-based interventions were no more likely to have improvement in pain at 3 months than those treated with placebo. In addition, fiber-based interventions did not reduce pain intensity. Although meta-analyses of low FODMAP or low fructose diets were not possible, the limited data available from the single studies of these interventions suggested they might offer some benefit, but the authors questioned the quality of the studies.
The researchers concluded that there was “moderate to low quality evidence suggesting that probiotics may be effective in improving pain in children with RAP.” They concluded that “Clinicians may therefore consider probiotic interventions as part of a holistic management strategy,” called for additional studies with improved protocols to evaluate these and other dietary interventions.
Summary and Clinical Applicability
Probiotics may improve pain in children with RAP. Fiber supplements do not appear to be effective. Clinicians may consider probiotics as a management strategy for RAP.
http://www.clinicalpainadvisor.com/abdominal-pelvis-pain/treating-pediatric-recurrent-abdominal-pain-with-probiotics/article/655570/

